Are There Lactation Meds For Moms Who Don’t Produce Enough Milk?
share this post
There’s a saying in business, “The riches are in the niches” and in most cases it appears to be true. Drug companies, however, don’t appear to think so when it comes to moms who can’t produce enough milk to breastfeed, a number that runs upwards to 5% of new moms who can’t make enough milk for their babies.
The highly marketed and insatiably supported campaign for “breast is best” has willed us all to be breastfeeding moms. Breastfeeding is praised, revered, and advocated for on national and social platforms. Science backs it as the “gold standard” for infant nutrition.
It’s not so much a mother’s sacred and private act as the nowadays standard for healthy motherhood. And good businesses know how to capitalize on a cultural manifesto. We’ve seen the “baby needs the boob” t-shirts, the colorful breast pump accessories, the animal-plaid Boppy pillows, and the beautifully fashioned cover-ups. I’m just wondering when big pharma is going to show up to the party.
I’m a pro-breastfeeding mom. Whether brain-washed by culture or because I tend to lean towards the most natural thing, I wanted to breastfeed my baby. Not only did I want him to have breast milk, but I wanted that special experience of nourishing him through breastfeeding. But I don’t like the powerlessness that some moms face when when breastfeeding doesn’t work out.
I remember the night I read this article from CNBC a month after I stopped trying to breastfeed my son. I struggled privately all the time thinking about how he wasn’t getting what was “best” for him. With access to all manner of resources and tools, I was equipped for breastfeeding - I just couldn’t make it work. It was like climbing a mountain of mud in flip flops.
Between a persistently bad latch, moderate to severe GER (acid reflux), and chronic low milk supply, I could not teach my son to nurse from the breast successfully. I kept thinking, You don’t need to convince me! Breastfeeding is the healthiest option for me and my baby. And you know what, I want to save money, too. I believe you, American Academy of Pediatrics and government campaigns and lactation nurses and mom friends! I really want to do this; we just can’t.
There’s an unexpected consequence in all this - new moms are more stressed than ever to make breastfeeding work. The message we hear is that good mothers breastfeed, and it creates a lot of self-blame and doubt when we can’t make it work.
there is No specific medication designed to help with lactation - so moms improvise
The problem for many moms is not motivation - it’s that she can’t produce enough milk due to Insufficient Glandular Tissue or hormonal imbalances, or a lack of time needed to pump around the clock, or previous breast repair surgery that has affected nerve and tissue function, among other deterrents.
It seems that some of the money and energy for pro-breastfeeding campaigning - especially since that message has been well-received - could be redirected to the research and development of medications that help with lactation. But since there isn’t a medication specifically designed for moms who don’t produce enough milk, many women resort to other options.
A hormone called prolactin is the central hormone in milk production. In recent years, women began taking prescription drugs which increase prolactin levels as a side effect, determined to increase their milk supply. For example, domperidone (Motilium) and metoclopramide (Reglan, Maxeran), are dopamine-inhibiting drugs that treat intestinal disorders or nausea and vomiting caused by other prescription medications. There’s also metformin (Glucophage), a medication which stabilizes blood sugar, and should really only be used for mothers who are pre-diabetic or insulin resistant.
While many medical professionals claim there is no evidence that these drugs increase prolactin levels - and are not worth the risk anyway - many moms and lactation consultants refer to them as “wonder drugs” for making more milk.
These drugs do have side effects, so a mom has to weigh whether it’s worth it to potentially increase her milk supply. A side effect of Reglan, for example, is depression - for which new moms are already at high risk. Not to mention that it is not available for purchase in the U.S. (moms go through online companies or back channels), and it is very expensive.
There are herbal remedies for increasing milk supply, called galactagogues, which have varying levels of success among moms. It’s typically a concoction of supplements that moms take multiple times a day, and we don’t yet know how much of these supplements make it into breast milk. Moreover, they often cause intestinal discomfort and headaches when taken frequently. The most common supplements are fenugreek, goat’s rue, brewer’s yeast, shatavari, fennel, and alfalfa.
Most moms start out assuming that they will have enough milk, unless they’re already aware of a condition that might affect breastfeeding. By the time they recover from milk blebs and cracked nipples, they’re usually already supplementing baby with formula. If mom’s milk supply remains low, the bottle is much easier to feed from and therefore negatively impacts mom’s and baby’s breastfeeding relationship. (Think about the difference between eating crab legs and chicken. So much more work to eat!)
what is lactation failure and how do we handle it?
What often happens for moms is that they end up switching to formula or pumping what little milk they produce and giving it to baby through bottle feeding. The fact that moms are just supposed to move on from breastfeeding failure is a little absurd. It’s as Dr. Stuebe, a maternal-fetal medicine physician and breastfeeding researcher says, “With little knowledge and few treatment options, the physician is typically left telling a mother that she has lactation failure. Too often, that diagnosis is followed by some patronizing comment like, ‘It’s ok — I was formula fed, and I turned out fine.’
Consider that we spend more than $1 billion a year on Viagra to treat another type of reproductive malfunction. I suspect men with erectile dysfunction would not respond well to being told ‘We’re sorry, we don’t have a treatment for this important aspect of your reproductive and social well-being. But here’s an artificial substitute.’
If you search the database of federally funded medical research for lactation failure, there are only 9 studies listed, compared with 84 for erectile dysfunction. It seems that, as a nation, we simply don’t consider inability to breastfeed to be an important problem.”
So, why don’t companies dedicate more time, money, and research into creating a medication specifically for moms who can’t produce enough milk to breastfeed? Instead of a treatment option, we are left with a list of over 30 supplements, like the galactagogues I mentioned earlier, which still don’t directly increase prolactin levels and often cause gas, bloating, and stomach cramps.
I don’t want to be cynical, but is it because there’s not enough money in it? Moms only breastfeed for a relatively short amount of time - compared to men who may use erectile dysfunction medication for 10+ years. (Not to mention that the development of E.D. drugs is sex and pleasure-driven.) Other treatments that attract researchers and revenue are life-long medications or drugs used in hospital settings.
Dr. Stuebe goes on to ask, “Why do we accept that malfunction of a major part of reproductive physiology is untreatable, and that the acceptable solution is a synthetic substitute and a pat on the head?”
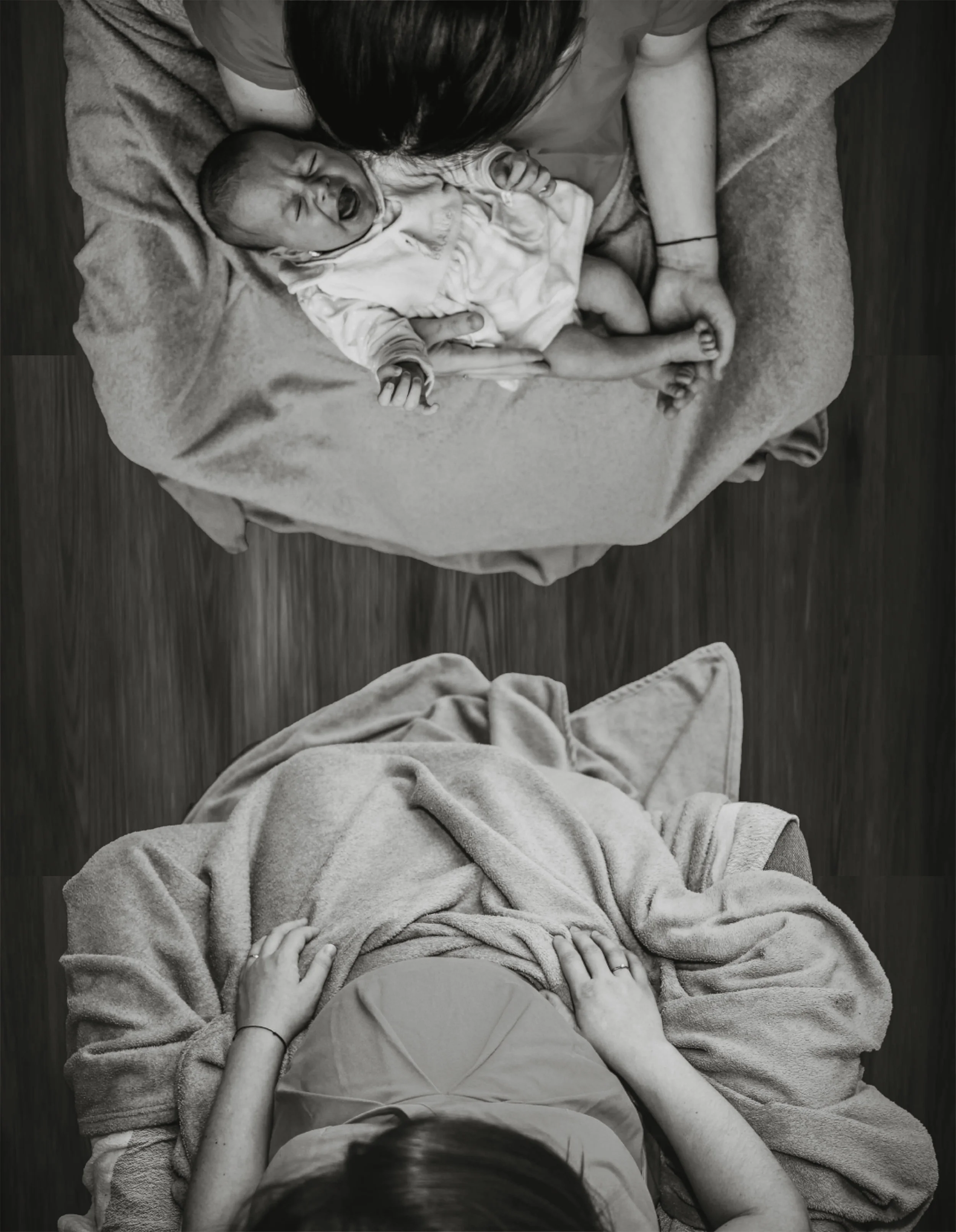
Not producing enough milk to breastfeed your baby is an important reproductive dysfunction that warrants R&D for safe and proactive medical solutions. A mom’s efforts - sometimes extraordinary - should be honored with endeavors towards real solutions rather than glossed over as a trivial and unfortunate circumstance. There’s also so much more to breastfeeding than milk, as this is a special time for bonding, skin-to-skin contact, and comforting between mother and child. It’s irresponsible to minimize something with such intrinsic value and positive health benefits. And it’s too common a problem to ignore.
Calls to action
Lactation specialists and similar clinicians need early intervention training to diagnose moms with milk production issues, whether due to IGT (insufficient glandular tissue) or another cause. The pro-breastfeeding agenda should not prevent skilled professionals from determining when moms are having real problems with milk production and getting the right support for them.
Moms need advocates in positions of power speaking on their behalf for organizations and major pharmaceuticals to find more funding and commit more time to creating a safe medication specifically designed to support lactation.
Research needs to uncover the specific reasons for lactation failure and development treatments to help moms meet their breastfeeding goals.
Moms need to be given more realistic goals from their lactation consultants once it is determined how much milk they can produce. Too much guilt and loss are a result of moms being told they can do it if they “hang in there” when they just aren’t able to produce enough milk.
As with any major change, we need to start by asking questions and advocating for progress.
The scientific and medical community has solved greater problems than this. It’s time to hone in on that niche of mothers who can’t breastfeed due to low milk supply and give them the richest breastfeeding relationship possible.